Revealed: Bristol care workers speak out amid confusion and scramble for PPE during covid-19 outbreaks

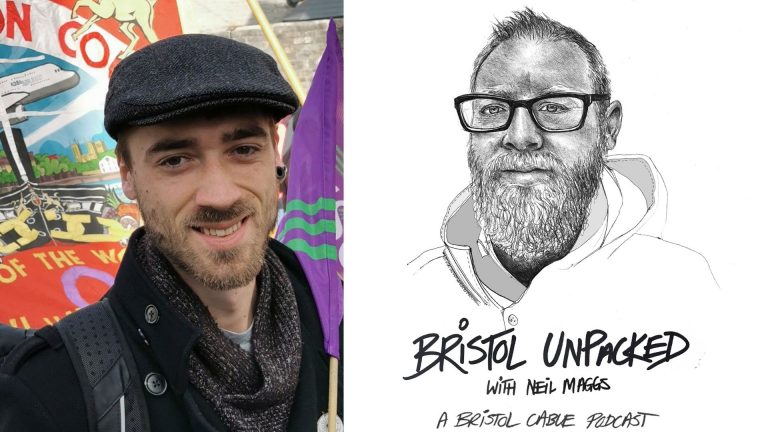
Illustration: Rosie Carmichael
Care workers doing 60 hour weeks are facing shortages and confusion on PPE as it emerges that 60 residents have died from coronavirus in two weeks at Bristol care homes, a Cable investigation has found.
In one Bristol care home, five residents had tested positive and four showing symptoms had died, but further testing was not made available. Brunelcare, another major care provider in the city, had to “fight hard” with Public Health England (PHE) to get more residents tested and, unable to access national supply chains, came within 24 hours of running out of PPE.
Speaking to the Cable on the condition of anonymity for fear of losing their jobs, care workers have revealed not being allowed to wear face masks while caring for people, raising questions about whether PHE guidance is being implemented correctly.
“Last Friday, I had 24 hours left of masks. You can’t continue to give care if you don’t have the right PPE, because I have a duty to my staff”
On Tuesday after weeks of speculation about how widespread the pandemic has been in social care settings, data was released showing the number of deaths from coronavirus in Bristol care homes had reached 60. Exactly the same as in the BRI and Southmead Hospitals over the same period.
The figures for those who passed away in the two weeks between 10 and 24 April is three times higher than before the virus gripped the sector. However, care home staff have now told the Cable about the difficulty in certifying deaths during the crisis, sometimes without the support of a GP, which suggests the true toll may be even higher.
Despite repeated promises by local and central government, care workers are also struggling to access testing, which has meant providers are paying extra to hire agency staff while employees are self-isolating. In a sector racked by years of austerity, this is placing even more financial burden on providers who may struggle to survive the crisis without further financial support from the government.
As families and residents are kept apart for hygiene reasons, workers in a sector renowned for poor pay and conditions have been working as hard as ever and filling in gaps while covering for colleagues, even while managing health conditions themselves. With so many workers poorly paid or on zero hours contracts, the Bristol branch of the union UNISON has said the pandemic presents an opportunity to reassess the value of care work in society.
Tests come back positive, but no more available
The outbreak in the local care sector is extensive, with the council working with 20 care providers with confirmed or suspected cases of Covid-19 as of 19 April. This may now be higher, though inconsistent testing remains an obstacle to assessing the true scale of the virus among thousands of local care home residents.
In the Bristol care home where four residents with symptoms have died, there were 15 ill residents with suspected coronavirus. However, a source told the Cable that although all five testing kits that have been provided to care homes came back positive, no further testing was available to confirm the extent of the outbreak. At the time of the positive test results, staff at the home were working without PPE. As staff and residents waited for about a week for an order of PPE to arrive, the virus continued to take its toll. “Two were people who went into respiratory distress in the morning and were gone by the evening,” said one worker.
Oona Goldsworthy, the CEO of Brunelcare, which runs three homes in Bristol, has had similar struggles around testing. “Initially when residents had symptoms, we were getting them tested, then for two weeks Public Health England said they couldn’t test any more, we kicked back against that and did get tests. There hasn’t been a situation where we’ve been without testing, but we’ve had to really fight for it.”
Health secretary Matt Hancock said two weeks ago that all ill residents would get tested, but last week PHE admitted that this wasn’t yet available. The government announced on Wednesday that testing is being rolled out for all care home residents, but it remains to be seen if that has come into force.
Bristol City Council did not know if extra testing had been made available for residents when outbreaks had occured. Neither Public Health England or the Department of Health and Social Care answered our questions about this.
A council spokesperson said: “Bristol City Council officers from Adult Care and Public Health have worked alongside community health colleagues to provide support including access to information and advice on matters such as infection control, accessing staffing and nursing practice, practical help with emergency PPE provision and general support for managers during a difficult time.
“We are working closely with our care homes to support residents and their families at this difficult time and the council is currently finalising additional payments to help care homes with the financial burden.’’
Mixed messages, and fear of speaking up
About three weeks ago, PHE changed the guidance on wearing masks, Goldsworthy said. “The advice went from very strongly that we shouldn’t be wearing masks to a particular type of fluid repellant mask. They weren’t in supply. Suddenly, you’ve got the whole of the care sector, GPs, community nurses, hospices didn’t have this and suddenly had to gear up for it overnight.” The change in guidance presented a major challenge, given that the charity now has to go through 2,000 masks a day.
PHE guidance now states that fluid repellant face masks and eye protection should be worn continuously apart from when eating, drinking, or taking a break. It appears that the first major change towards wearing face masks in a care setting was on 8 April, even though Covid-19 deaths are recorded in Bristol care homes as early as the last week of March.
Share this investigation
One care worker, who supports elderly people in their homes, said that even after speaking to his managers there was a “grey area” about whether he should be wearing a mask. Over the last month, he has worn a homemade mask, but felt unable to speak up because of job insecurity.
“Last Friday, I had 24 hours left of masks,” Goldsworthy said. “You can’t continue to give care if you don’t have the right PPE, because I have a duty to my staff.”
Goldsworthy resorted to making an appeal on BBC news, which helped them get a few more suppliers. “PHE are coming out with the advice, but there aren’t the resources to match that advice. For the resources not to match the science is really scary.”
The pandemic has exposed a weakness in how the care sector syncs up with the NHS, says Goldworthy. “As care providers have been left to our devices. There’s been no support. Local authorities have tried to get us what they can but they’re in the same position. Because we’re not part of the NHS, we don’t get any central support.”
Professor Martin Green OBE, CEO of Care England, said there had been “huge difficulties” in accessing national supply lines, which were initially requisitioned for the NHS. Green also said that care providers had been “bemused” by PHE’s guidance on how and when to use PPE.
A care worker in a nursing home said she was prevented from wearing a face mask as late as 17 April, because there hadn’t been confirmed cases. Fearing for her safety, she quit the role. Steve Mills, a local union rep for Unison, said this picture was not uncommon across the sector, with other large care providers reportedly even preventing workers with health risks from wearing face masks.
“I’ve seen the whole spectrum,” he told the Cable. “With some care companies being very proactive and supportive, and the other end where they really are putting people at risk – people who have underlying health needs are still being expected to work.”
The Cable spoke to one carer who works in a rehab centre for men with a mixture of mental health issues. They had been supporting a patient with underlying health issues, who had coronavirus symptoms for a number of weeks – a cough, struggling to breathe and a very high temperature. However, the patient was only tested last week and staff were not recommended to wear face masks until this week. “It’s a matter of too little, too late,” the worker said.
Working more than 60 hour weeks, they are one of tens of thousands on a zero hour contract. Due to insecure employment they felt unable to speak up because of fears of not being offered more shifts. They added that at one stage the ward didn’t have a working thermometer, and on two occasions didn’t have cleaners over the weekend because of staff absence.
Fighting a virus blind
Goldsworthy said Brunelcare staff are now being tested, but of all the other care workers the Cable spoke to none had been tested or knew anyone who had. On Wednesday, the government announced that NHS and care home staff would be tested with or without symptoms, but the capacity of the regional testing centre at Bristol Airport is unknown. The Department of Health and Social Care said it is not releasing this information.
A nurse, who has been working up 70 hours a week in a care home where a number of staff are off sick, said: “We need more testing, and we need testing of the staff so they can get their regular staff back and reduce their agency bill, it’s enormous.” As the UK faces up to a death rate among the highest in the world, the nurse spoke of the need for tests to keep these exhausted key workers on the front line. “Testing would also make people feel a bit more confident, I think.”
You can also hear from a Cable member what it’s like having a relative in a Bristol care home, and read an in-depth look into what the undervalued social care sector needs in order to improve after the pandemic.
Contact us condifentially with any information about how Bristol’s care homes are coping during the crisis. Get in touch by emailing: matty@thebristolcable.org.